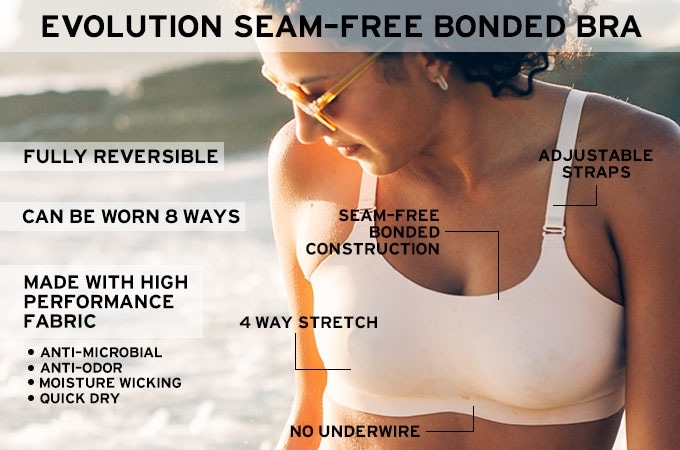
Handy tips for the inconvenient underbelly of DCIS breast cancer surgery and radiation treatment1/10/2017 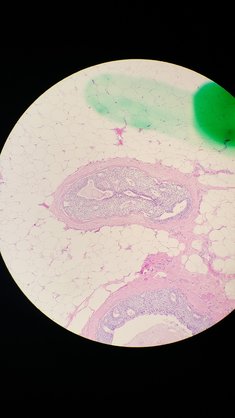 Some of my DCIS cells. Some of my DCIS cells. At the end of last winter, I started thinking about not getting my annual mammogram. I mean, my mammogram had been the same for 30 years. Three little round calcifications that never changed. Why would things change now? Several of my friends never get mammograms, citing statistics about radiation exposure or over treatment of early abnormalities. Maybe I’d just skip that extra dose of radiation, give my increasingly old body a little break. Breast cancer has popped up with some frequency in my family—my sister & a couple aunts, all at younger ages than me. This stuck me in a high-risk category over the years. But had I aged past the danger? I mean, I have aged past the need for a pelvic exam. I’m unvaryingly healthy, if you don’t count the removal of my malfunctioning appendix and gall bladder, or that worrisome lump on my thyroid. I rarely even get a cold, recover handily from banged bones and abused ligaments, and have always thought of myself as stronger than the average bear. When I got the reminder postcard in the mail one chilly March day, I hesitated. But before I throwing it in the recycling, I decided to Google around about the age to quit mammograms. Of course, I found that the risk of breast cancer rises with age—"rates are highest in women over age 70." Actually the risk of all cancers rises as we grow older because of the aging of our cellular system, but that's neither here or there. Being 66 years old, I made the appointment. This time things weren’t as routine. First there was the need to redo the scan. Then there was the announcement that I had some abnormal cells, and a biopsy was scheduled. Then the meeting with grim-faced doctors. I had DCIS. Ductal Carcinoma In Situ. A Stage 0 cancer that had not spread anywhere. A spot about the size of a thumb. A tiny, spot unable to be felt even by the most experienced medical fingers. Stage 0? Not Stage 4. Not You-Aren’t-Dead-But-Let’s-Do-Surgery-Chemo-And-Radiation-On-The-Way-To-Your-Grave cancer. OK! But then, they started talking about doing a double mastectomy and rebuilding my breasts with other body parts. “We treat this the same way we would a more advanced cancer,” they said with authority. Fast forward a month or so, and the size-of-a-thumb spot (newly imaged with more fancy equipment and evaluated by big-city radiologists up the road) now is the size of a fist. Still, the news is good. I don’t have the dreaded BRCA genes that give about a 50-50 chance of developing breast cancer. And no mastectomy. Just digging out the nasty cells in a lumpectomy followed by oncoplastic surgery to fix up my breast and a reduction get the other one to match. “How about perky little C-cups?” the oncology surgeon said merrily as she glanced at my generous breasts with some disgust. Fast forward to the end of May. My new, perky little C-cups look like a gruesome, bloody patchwork quilt as I perched unsteadily on the edge of a whole universe of unmentioned agonies admist the cheerful reports than the area of abnormal cells was actually the size of a pinkie fingernail, but that it was an aggressive, more dangerous sort of DCIS. Anyway, here, almost 8 months since my surgery, I am grumpily grateful for the removal of these potentially very nasty cells and hope I get to keep my perky little C-cups; that they don't get sliced off at some point in the future. I could have gone happily my whole life with the inconveniences of big tits, but since it's done, why not enjoy the benefits? My clothes fit better, I look better, and all that jumping in my Zumba class is easier. But mostly, I think about other inconveniences—the side effects, and discomforts of the treatment I received. The looming possibility of my cancer returning has always seemed nebulous and distant, nothing compared to the immediacies of opening incisions, painful scar tissue, or persistent itching. My oncology doctors don't give a fig about these little things; their focus is on keeping me cancer-free. But I think about it every day and have since I woke up from surgery. I have given up countless hours of my life Googling and wasted an amazing amount of money trying to find solutions while wandering the DCIS lumpectomy oncoplastic radiation wilds. I know I am not alone in my search for an easier post-breast cancer surgery and radiation treatment life. Everywhere I went on the internet, women were out there alone trying to sort out what was going on and what to do. So I thought I'd put together some of the things I learned. I hope, if you are in a similar situation and you find your way to this page, these tips might help you. For some items I have provided Amazon links to buy, I do not make any money off these recommendations. If you get to feeling alone, you can always sign up on the Real Self website where women share absolutely everything with photos about cosmetic surgery, including breast cancer surgery, and various physicians comment. There are many women out there who blogged throughout their treatment (not me!) Here are 3 good ones to start with, good pix: 1 The Banshee. 2 I have Breast Cancer --Say What? 3 My So-Called Breast Cancer.  Nope, don't put the cami over the bra. Turn it inside out and put it under the bra. Nope, don't put the cami over the bra. Turn it inside out and put it under the bra. Before surgery Buy a notebook, bring a friend, organize everything, Then ask, hunt, ask. Write down your questions. Write down their answers, or better yet, bring a friend to do it so you can listen. Ask every doctor the same questions (I got different answers). Throw away the folders they give you and make your own. My file categories: contacts, patient ed, articles, onco surgery, plastic surgery, radiation onco, clinical trial, genetic testing, maps/directions, test reports, notes, diet. Consider writing up everything you heard when you get home from appointments. It will help cement the information in your brain and generate questions to Google and ask. One of the most important jobs you have as a patient is to ask, hunt for information, and ask again. Doctors have a low common denominator of standard information that they dole out. If you ask, and ask, and ask good questions, they respond with more and better information. The challenge is keeping track of everything and sorting through the garbage that's online. Get advanced care: It is worth it to have an oncoplastic breast surgeon and an oncology breast surgeon working together versus a general surgeon. If you live in the boonies, go to the big city and get yourself a top-notch team. Surgeons who only work on breast cancer are boatloads better than those who do it part time. I had a less invasive, more cosmetically pleasing surgery than the one proposed locally and was able to come home without drainage tubes. However, I did my daily radiation locally and got a less invasive technique because I did. I was enrolled in a clinical trial that my local center was not participating in, but upon my asking, they were able to be included. So ask, hunt, ask. Remember you have choices! Don't let the system rush you. Get your drugs before being released from the hospital. I made a big mistake here. The evening I was released from the hospital, they handed my daughter written prescriptions for pain. Unknown to me, the diazepam had to be pre-approved by the insurance company—so the cost wasn’t covered when we got to the drug store. The Percocet wasn’t in stock, and we had to drive around to get it from the only CVS in town that had it, barely making it there before the store closed while the pain meds I'd taken long ago at the hospital were wearing off. This is not how you want to spend your time immediately after being released from the hospital. I haven't tried it, but I have heard from others that you can get these prescriptions filled in advance. Know that some pain medications can only be ordered with handwritten prescriptions. After surgery, I realized I had only gotten a couple days of pain meds, with no refill. The new prescription had to be picked up in person. My doctors were 60 miles away in another city. Don’t let this happen to you. Read the prescription! Through the quick thinking of a nurse, my local primary care doctor was able to write a prescription. Sort out pain medication plans in advance. My oncology surgeon and my plastic surgeon had completely different ideas about what pain meds I needed. One thought I could get by on ibuprofen, the other thought I needed stronger medicine (and I DID). Don’t get in the middle. Have this discussion before surgery and get your meds before you leave the hospital! My discharge prescriptions were written by the doc preferring ibuprofen and HO BOY was I sorry. It was a mess. Prep your house before you leave for surgery. Make it easy on yourself. You’ll be hungry and you won’t want to cook. Freeze or buy single servings of food that you like. Be sure to have plenty of fiber on hand to offset the constipation of pain meds–bean soup, dried fruits, bran cereal. You won’t want to lift anything heavy. So buy smaller sizes of milk etc. and put out small pots and pans. You’ll want to set up your bathroom and bedroom too. The American Society of Plastic Surgeons has a worthy guide with lots of good ideas. Download it. Hire housekeepers. Unless you have someone else to clean your house, find someone to hire. You won't be lifting, pushing, or stretching for awhile. Be healthy before surgery. My hospital assumes that everyone eats a poor diet and routinely recommends a few days of meal-replacement, immunonutrition IMPACT ADVANCED RECOVERY® beverages before surgery. I was able to avoid these god-awful drinks by reading to the pre-op staff from my food tracking app what my daily levels of protein and other nutrients were. Have loose, front button clothes. PJs and big shirts! Get ready to sleep on your back. I'm not a back sleeper, but I can do it. I decided to buy a fairly expensive foam wedge to help me. I hated it. For me, a collection of pillows, supplemented by my easy chair, worked the best. So if you buy a wedge, get it somewhere you can return it. Get a boatload of camisoles. I came home in a surgical corset that was never comfortable. It bunched up under my breasts killing my incisions. I quit wearing it early, but needed support to keep the weight of the perky little C-cups from pulling on the incisions. Any bra-like garment hurt. Not wearing one hurt. I tried wearing a giant front-closing sports bra from Wal-Mart with a cami on top to keep things stable (see pic). But that hurt too much. So I turned the cami WRONG SIDE OUT so the seams didn’t rub the side incisions and wore it under the bra. Later, I abandoned the bra and put on two camis, fold the top one up to give bra-ish support without hurting tender incisions. If you decide to try sports bras, look for the bigger sizes—they are really tight! My needs changed over the months. When I was doing radiation, soft was essential. When I was trying to reduce my lymphedema, compression was important. When you are ready for a bra, get this one!!!! It took me almost a year to find a comfortable bra that didn't irritate the heck out of the side incision of my radiated breast. There are many bras out there that say they are seamless, but they aren't. This one is. Not only that, it's cute. It molds to your body, 60% nylon, 40% spandex. Just enough compression to make my lingering lymphedema better. They rock! 8-in-1 Evolution Bra by Knixwear. The best camis
After surgery Your incisions might split. At the “T” where the incision from the nipple meets the incision running under your breast, and along the bottom incision. Mine did this at about 3 weeks after surgery just when I thought things were looking pretty good. It was nasty surprise that didn't surprise my surgeon who was never worried about it but who also didn't warn me it might happen. Slowly the seeping holes did close up on their own. I saw online that some women get huge holes that somehow manage to heal. Now I have weird, thick scars where this happened. Keep the glue. I had a black line of glue on my incisions that was very uncomfortable as it aged. Don’t pull it off. Just be uncomfortable. It's supposed to come off naturally after 3 weeks, but mine wasn't. It drove me crazy and I picked at it. I suspect this may have caused the opening of my incisions. Don't be like me! You may get a huge lump where your lumpectomy was. Mine feels like a hard handball. If you get one, insist on having it imaged to discover if it is a seroma (fluid) in the surgical cavity, lymphedema, or scar tissue. Mine is fat necrosis—scar tissue. Damaged, fat tissue that lost its blood supply and died, and then got fried by radiation, creating a hard cap. I massage mine hard. Have been told to use warm compresses for 30 minutes every 4 hours. But who can do that? Plus, after radiation, fibrosis can develop, a hardening of the breast that irreversible. It's important to keep that hardening tissue moving or it will harden even more. See below about massage. Live a cruciferous life. There’s some convincing data that cruciferous vegetables (cabbage, kale, broccoli, arugula, brussel sprouts, radishes, cauliflower, etc.) help to metabolize estrogen and generally protect against cancer. Cruciferous veggies are high in glucosinolate that enhances the elimination of carcinogens before they can damage DNA, or by altering cell-signaling pathways in ways that help prevent normal cells from being transformed into cancerous cells If you had an estrogen-related tumor. It’s so easy to add a helping every day. Read about it. Dealing with radiation  Targets, scars, radiation-ready. Targets, scars, radiation-ready. Protect your heart and lungs, get breath-hold radiation therapy. Especially if your left breast is being radiated. This technique significantly lowers the radiation dose to your lung and heart. When you hold your breath it pushes most of your heart and lungs out of the way of the radiation beam. It 's a big deal. Find a place that offers it. Many of the bigger, busier radiation centers don’t offer the technique because it slows the patient flow. Patients have to learn how to hold their breath for 20-30 seconds guided by a recorded voice. It was easy for me to do and the voice at my center was so soothing that I looked forward to hearing her speak gently to me, "Hold your breath. Breath. Hold your breath. Breath." Read more about it.  Big lymphedema pores, thick healing incision, midway through radiation about 3 months after surgery. Big lymphedema pores, thick healing incision, midway through radiation about 3 months after surgery. Bookend treatments with positive things. Radiation is just a sucky thing to do. Try to put it in somewhere in your life that’s not too bad. I tried to stay as active as possible through the recovery from surgery and during radiation by walking, but it was a challenge because of the jiggle factor on the healing incisions. It was better when divided up the walk into smaller segments throughout the day. A soft indoor track is nice too. So I took a walk, listening to a book every day right before my treatments. After the treatment, I looked forward to settling into my easy chair when I got home with a Spicy V8 Power Smoothie of my own concoction. The walking upped my energy to fight fatigue and the smoothie made me feel as if I was supporting my blasted body. I drank one of these after every radiation treatment, and plan on drinking one every day for the rest of my life. It's nice to pour all those vitamins into your body without the sugar of those fruity smoothies. Try it: Whir up a cup of Spicy V8 (or some other tomatoey juice) with a handful of baby greens. Sometimes I add sprouts, sauerkraut, nutritional yeast. Unscented goat-milk soap. My doctor recommended an unscented, moisturizing bar soap like Dial to wash with during radiation, but I couldn’t find any in the stores. I COULD find bars of unscented goat-milk soap at the local BloomingFoods co-op and that worked great. Calendula lotion. Before, during, and after radiation, I diligently followed my radiation oncologists orders to slather myself with various lotions, including calendula lotion (not ointment, cream or gel). I could find the lotion in local stores but it was super expensive. Much cheaper at Amazon. The radiation center staff and doctor told me that my skin stayed in better condition than many because lots of women just don't put the lotions on. Have thick scars? Get massage. My breast that had the abnormal cells, where “all the work was done” started out with a very thick incision scar. It got much thicker during radiation. And, I read online about deep tissue massage to lessen the thickness and loosen the skin and got confirmation from the massage therapist at the radiation center. After much whining and asking every one of my doctors, I was able to get a referral (instead of paying out of my pocket) from my plastic surgeon to physical therapy at the local lymphedema clinic for massage. This is not regular massage, you need to get it from someone specially trained in post-radiation, post-surgical massage. It really made a difference, but I still have thick, uncomfortable regions that I continue to massage myself. Next I’m trying therapeutic ultrasound*; the oncology nurse practitioner recently gave me a referral, wondering why I hadn’t gotten one before. Again: ask, hunt, ask. Be sure to watch out for fibrosis, the tissue scarring and thickening that can show up even ten years after radiation. What starts out as tenderness and redness turns into firm, hard, uncomfortable mass. *UPDATE: It turns out that radiated breasts have compromised vascular systems. That means ultrasound massage cannot be done. This was discovered when the ultrasound massage referral was mistakenly sent to the physical therapist who did the manual massage on my scars. She contacted the oncology nurse practitioner who didn't know this! The NP confirmed with other PTs and cancelled the ultrasound referral. Geez! Thank heavens for that mistake that prevented a mistake. Even if you don’t have a lymph node removed, you might get lymphedema. Both surgery and radiation can cause the formation of more (!) scar tissue that blocks the flow of fluid in lymph vessels and nodes. My radiated breast has a mild case of lymphedema that keeps things sore; I'm told it may never go away. If you see big pores in the skin of your breast, that’s the sign that you’ve got it. Ask your doctors about decongestive breast massage and Google it. Here’s a good video. Lymphedema might show up days, weeks, or months after radiation. Get a referral if you can to a therapist at a lymphedema clinic. See if you can get a foam form to help move fluids and prevent fibrosis. My physical therapist at the lymphedema clinic made me a form from open-cell, low density foam covered with a gauzy sleeve that I wear at night. Magically it helps move the fluids in my breast (both vascular and lymph) and works like massage to reduce the scars and fibrosis. The radiation may have permanently altered both the vascular and lymph pathways of my breast, and I may end up wearing this for the rest of my life. But it sure makes a difference. I thought I was well past needing it and quit wearing it and things went down hill with more swelling and shooting pains. She also made me a foam chip bag to wear that helps fight the fibrosis more aggressively. If you can't get help, you can hunt down Schneider pads and Schneider packs online. Exercise instead of hormone treatment. My medical oncologist was okay with me not taking tamoxifen. What with my substantial round of radiation, huge margins, and stage 0 cancer, she felt I was adequately protected. When I mentioned that I had hired a personal trainer to design a set of routines to bring back my muscles from the ravages and weakness of surgery and recovery, she casually said that if I stuck with it, exercise provided as much protection as hormone therapy! Why don’t they promote this? Why did I only hear this when I brought it up? Anyway, several weeks into my new exercise routines (upper back, balance, core + 2 miles walking & Zumba), I can felt my old self returning. Or is it a new self? Vitamins to give your poor zapped breast help revitalizing. I don't know if it makes a difference. but hey! Why not? A friend of mine advised me to do a round of B complex, beta carotene, vitamin E, and vitamin C just as soon as I finished radiation. I did. And then my breast grew more sore about four months later from lymphedema, so I'm taking B complex and vitamin E for at least another year. Along with rutin, which I hope will boost my breast's crippled vascular system.
3 Comments
|
Inside
|




 RSS Feed
RSS Feed